HCI Community Health Needs Assessment Guide
Define and Understand Your Service Area
Prior to identifying the most significant community health needs, you'll need to define and understand the demographics of your service area.
Click on an item below for details:
-
Step 1: Define Service Area
-
Geography
What zip codes, counties and cities are part of your service area?
- and/or -
Specialized Target Population
Does your hospital focus on serving a specific population (e.g., children, women, or the elderly)?
Important Note for Hospitals: A hospital facility may not define its community to exclude medically underserved, low-income, or minority populations who live in the geographic areas from which the hospital facility draws its patients (unless such populations are not part of the hospital facility's target patient population(s) or affected by its principal functions) or otherwise should be included based on the method the hospital facility uses to define its community. In addition, in determining its patient populations for purposes of defining its community, a hospital facility must take into account all patients without regard to whether (or how much) they or their insurers pay for the care received or whether they are eligible for assistance under the hospital facility's financial assistance policy. IRS Community Health Needs Assessment Rule 12/31/14.
-
Step 2: Research the Service Area's Demographics
-
Consider describing the following:
- Population
- Under 5
- Under 18
- Over 65
- African-American/Hispanic/Asian/Pacific Islander/White
- Language other than English spoken at home
- High school graduates and bachelor's degree or higher
- Median household income
- Persons below the poverty level
Explore Demographics Dashboard
-
Step 3: Identify Zip Codes with High Socioeconomic Need
-
-
Tips for the Final Report
-
- Provide a short justification for your selected service area (e.g., "We selected Main County as our hospital's service area because over 70% of our patient population resides in this county.)
- Include charts and visuals
-
From the IRS
-
In defining the community it serves for purposes of paragraph (b)(1)(i) of this section, a hospital facility may take into account all of the relevant facts and circumstances, including the geographic area served by the hospital facility, target population(s) served (for example, children, women, or the aged), and principal functions (for example, focus on a particular specialty area or targeted disease). However, a hospital facility may not define its community to exclude medically underserved, low-income, or minority populations who live in the geographic areas from which the hospital facility draws its patients (unless such populations are not part of the hospital facility's target patient population(s) or affected by its principal functions) or otherwise should be included based on the method the hospital facility uses to define its community. In addition, in determining its patient populations for purposes of defining its community, a hospital facility must take into account all patients without regard to whether (or how much) they or their insurers pay for the care received or whether they are eligible for assistance under the hospital facility's financial assistance policy. In the case of a hospital facility consisting of multiple buildings that operate under a single state license and serve different geographic areas or populations, the community served by the hospital facility is the aggregate of such areas or populations.
IRS Community Health Needs Assessment Rule 12/31/14
Analyze Secondary Data
This site contains a wide variety of indicators from national and state data sources that you can review and analyze to help in your community health needs assessment process.
Secondary data refers to data about your community that has already been collected by various organizations. Much of this data is available for you to access on this site. A strong secondary data analysis allows for an objective start to looking at the health needs of your community and can help inform your community input gathering.
Click on an item below for details:
-
Step 1: Compare to Other Locations
-
COMMUNITY DASHBOARD
Depending on your site's geography and availability of the data from the data source, indicators may compare to other state counties, U.S. counties, state value, or U.S. value. You may wish to compare to a single location or multiple locations. Use the Build a Dashboard tool to select the comparison(s) you wish to view.
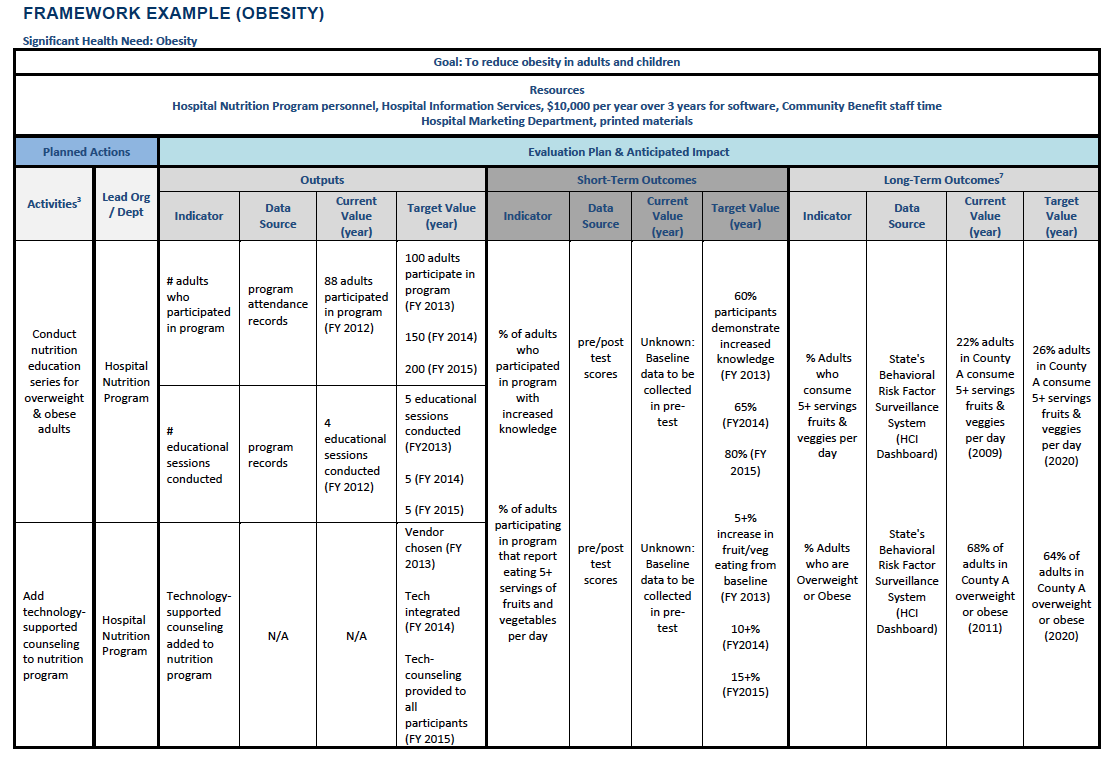
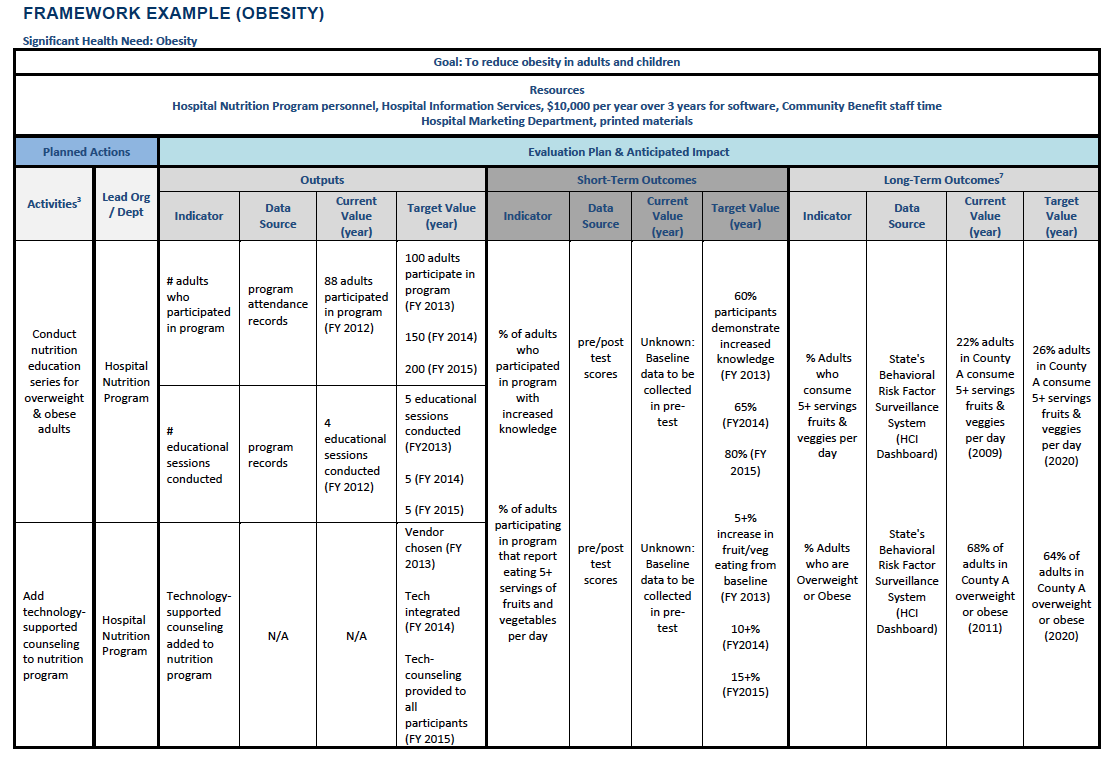
 If comparing to other counties, these indicators will have the red, yellow, and green divided gauge. When the needle is in the green, he selected county’s value is the top best half (50%). When the needle is in the yellow, the selected county’s value is in the bottom worst half (50%). And when the needle is in the red, the selected county's value is in the worst quartile (25%) of all counties.
If comparing to other counties, these indicators will have the red, yellow, and green divided gauge. When the needle is in the green, he selected county’s value is the top best half (50%). When the needle is in the yellow, the selected county’s value is in the bottom worst half (50%). And when the needle is in the red, the selected county's value is in the worst quartile (25%) of all counties.
 If comparing to a state or national value, these indicators will have a diamond-shaped single value icon. The arrow in the icon indicates if the indicator value is higher than, lower than or relatively equal to a state or national value. A green-colored icon represents the indicator value is better than the comparison value. A red-colored icon represents the indicator value is worse than the comparison value.
If comparing to a state or national value, these indicators will have a diamond-shaped single value icon. The arrow in the icon indicates if the indicator value is higher than, lower than or relatively equal to a state or national value. A green-colored icon represents the indicator value is better than the comparison value. A red-colored icon represents the indicator value is worse than the comparison value.
From the indicator detail page, you can easily save the chart that displays all location types by clicking on the 3 horizontal lines or by selecting download CSV to save all available location data.
-
Step 2: Compare to Healthy People 2030
-
HEALTHY PEOPLE 2030
Healthy People 2030 objectives are set by the US Department of Health and Human Services. These nationwide targets provide a benchmark for all communities to work towards.
View Healthy People 2030 Tracker
-
Step 3: Compare to Historical Data
-
TIME TREND
It is important to know how your community is changing over time. From a customized or curated dashboard, you will see a Prior Value of an indicator which compares to the previous measurement period and the Trend over Time which compares to a multi-year trend. From an indicator detail page, you can also view the Change over Time graph to see changes for that indicator's value over several time periods.
-
Step 4: Identify Disparities
-
IDENTIFY DISPARITIES
This dashboard allows you to view all breakout data, when available, for all indicators at once to find race/ethnicity, gender or age disparities. Consider using the Index of Disparity method to summarize disparities across groups and indicators.
Find Health Disparities
SOCIONEEDS INDEX® SUITE
You may also want to consider geographic disparities. Social and economic factors are well known to be strong determinants of health outcomes. Use the SocioNeeds Index® Suite to explore which locations (e.g., counties, zip codes, census tracts) in your service area have the highest relative socioeconomic need for a range of topics.
Find Geographic Disparities
Quick Tip: Understanding and identifying health disparities is a key step in the community health improvement process. Even if your community as a whole is meeting targets and performing well, health disparities within your community can still exist. It is necessary to understand the root causes of these disparities to successfully address and reduce them moving forward. Learn more at NACCHO's Roots of Health Inequity.
-
Step 5: Establish a Method for Your Analysis
-
In order to standardize and make your needs assessment replicable in the future, it is important to establish a clear method of how you identified community needs in your secondary data analysis. Clearly explain what criteria/methodology you used to identify your community needs.
Sample Method
"In order to determine our community needs, all indicators were analyzed on the following criteria:
- Is the indicator in the red or yellow?
- Is it failing to meet the national HP2030 or local target?
- Is it trending in the wrong direction?
- Is there an apparent disparity?
If the answer to any of these question is 'yes' the indicator was identified as a need. Once indicators were identified they were grouped and examined by topic area. These topic areas were identified as community needs."
-
Tips for The Final Report
-
METHODOLOGY SECTION
In the methodology section include information about where and when you accessed the secondary data. Also include any parties with whom you collaborated or contracted with for assistance in conducting the secondary data analysis.
Sample Text
The secondary data was collected and analyzed through www.sitename.org, a web-based community health data platform developed by Conduent Healthy Communities Institute and sponsored by General Hospital. The site brings non-biased data, local resources, and reporting tools to one accessible, user-friendly location. The site includes a comprehensive dashboard of over 100 community indicators covering over 20 topics in the areas of health, determinants of health, and quality of life. The data is primarily derived from state and national public secondary data sources.
APPENDIX SECTION
In the appendix make sure to include a list of data sources that you used including source name, URL of data, and measurement year. If you have administrative privileges, you can download all indicator information (including data measurement year and source name) in CSV format.
-
From the IRS
-
A hospital facility's CHNA report will be considered to describe the process and methods used to conduct the CHNA for purposes of paragraph (b)(6)(i)(B) of this section if the CHNA report describes the data and other information used in the assessment, as well as the methods of collecting and analyzing this data and information, and identifies any parties with whom the hospital facility collaborated, or with whom it contracted for assistance, in conducting the CHNA. In the case of data obtained from external source material, the CHNA report may cite the source material rather than describe the method of collecting the data.
IRS Community Health Needs Assessment Rule 12/31/14
Gather Community Input About Health Needs
Community input can be gathered through focus groups, surveys, meetings and interviews to integrate the community’s thoughts and perspectives into your community health work.
Click on an item below for details:
-
Step 1: Identify Community Input Sources
-
Consider speaking with the following people:
- Health Department Director/Officer
- Leaders of community-based organizations
- Teachers, principals, superintendents
- Clergy
- Hospital Staff (Executives, Doctors, Nurses, Administrators)
- FQHC Staff
- Members of vulnerable populations or those that can speak on their behalf
Important Note for Hospitals:
The IRS requires that community input is taken into consideration from at least one representative of the state, regional or local health department; members of medically underserved, low-income and minority populations (or people that can speak on their behalf); and written comments from the previous CHNA.
-
Step 2: Choose Community Input Method
-
Here are four commonly used techniques for gathering community input (adapted from the University of Kansas Community Toolbox)
Before you start, make sure you have a clear goal for the type of community input and content you are seeking to obtain. For example you may be looking to:
- Identify data information gaps
- Understand the community's perceived significance of identified health needs
- Expand knowledge and gain insights on data findings
- Identify barriers to receiving care
- Identify resources in the community
Having a firm understanding of your end goal will help you determine a community input gathering method that's most appropriate.
An interview is an in-depth conversation between an interviewer and someone with knowledge of the topic. Interviews can be time intensive to conduct but can provide details and context to a topic that may be otherwise difficult to obtain. Interviews can be both structured (a defined set of questions) or unstructured (a fluid conversation).
- Pros: Detailed results - often times unexpected answers, inexpensive, choose who you want to speak with
- Cons: Good interviewing skills take practice, can be time consuming if choose to do many interviews
- Learn More
A focus group is a structured small-group discussion around a given topic. A trained facilitator leads participants through an open-ended discussion where people voice their opinions and are able to react to other people’s opinions.
- Pros: Yields many perspectives and opinions in a short amount of time
- Cons: Need a moderator with focus group experience
- Learn More
A survey is a quick and efficient way of gathering information from a large number of people. Creating online surveys are often free (we suggest Survey Monkey) and if desired can be statistically significant.
- Pros: Inexpensive, large number of people can give input, easy to distribute
- Cons: Results may only represent people who answer survey, low survey response rate
- Learn More
Public forums are well-publicized meetings where a facilitator leads a discussion around topics such as health issues and strategies to address them. Open to everyone, public forums allow people of diverse backgrounds to share their opinions.
- Pros: Attract diverse people; large number of people can give input
- Cons: Can be expensive (staff time), interviewer bias
- Learn More
Quick Tip: No single community input tool is the best. Pick the ones that make sense for your organization, skill set, and the results you want to achieve. Don't forget you can also choose a combination of community input tools, for example, conduct 5 interviews and a public forum.
-
Tips for the Final Report
-
- Include when, where, and how the community input was obtained and analyzed.
- Identify the names of the organizations that provided input into the CHNA and summarize the nature and extent of that input.
- Make sure to describe the medically underserved, low-income, or minority populations being represented by the individual or organization providing input.
- In the event a hospital solicits but cannot obtain input from a source described in Step 1, the CHNA report must describe the hospital's efforts to solicit input from such sources.
-
From the IRS
-
The IRS requires that community input must be taken into consideration for prioritizing significant health needs from the following three groups: a) at least one representative of a state, regional or local governmental health department with knowledge of the health needs of the community; b) members of medically underserved, low-income, and minority populations in the community served by the hospital facility, or individuals or organizations serving or representing the interests of such populations; and c) written comments received on the hospital facility's most recently conducted CHNA and most recently adopted implementation strategy.
IRS Community Health Needs Assessment Rule 12/31/14
Determine Significant Health Needs
Before you prioritize and identify the health needs that your organization will address, you'll first need to identify the significant health needs of your community.
To determine if something is a significant health need, you should set criteria that are applicable to your community. Be sure to use the results from both your secondary data analysis and community input to draft your list of significant health needs, which can be used during the prioritization process.
-
Example Criteria
-
- Several indicators are trending poorly
- Large disparities among different groups
- A root cause to several chronic conditions
- A common theme discussed by focus groups/key informants
- Identified as a significant health problem during community input AND value is in the red or yellow compared to other locations
- Affects large number of people
Important Note for Hospitals:
A hospital facility may determine whether a health need is significant based on all of the facts and circumstances present in the community it serves. In addition, a hospital facility may use any criteria to prioritize the significant health needs it identifies, including, but not limited to, the burden, scope, severity, or urgency of the health need; the estimated feasibility and effectiveness of possible interventions; the health disparities associated with the need; or the importance the community places on addressing the need.
IRS Community Health Needs Assessment Rule 12/31/14
Understand Community Resources
An important part of assessing the health of your community is analyzing what activities are currently taking place to improve health.
Make sure you are aware of the organizations and programs in your community as you move forward with community health improvement activities. This can prevent the duplication of efforts and present opportunities for alignment or partnership.
Click on an item below for details:
-
Step 1: Start With What You Know
-
First, make a list of all the relevant programs that already exist within your organization or within your broader community. Consider using the local 2-1-1 resources or a community resource guide if available.
Quick Tip: While gathering community input, consider asking about programs and activities that they are running, participating in or would like to see. This will help create a more complete list of programs and resources that are out there and help to identify resource gaps.
-
Step 2: Reach Out to Organizations
-
Within your community there are other organizations working to improve population health. Consider reaching out to the following entities to see what activities they are currently implementing:
- Health Department
- United Way
- Non-profit community organizations
- School counselors
- Medical social workers
-
Tips for the Final Report
-
The CHNA report should include a description of the potential measures and resources identified through the CHNA to address the significant health needs. Focus on identifying resources that address your significant health needs first. Provide a high level overview of resources within your report, but consider listing all of the available resources or linking to existing resource guides in an appendix.
-
From the IRS
-
A description of the resources potentially available to address the significant health needs identified through the CHNA.
IRS Community Health Needs Assessment Rule 12/31/14
Evaluate Your Progress to Date on Past Health Priorities
Take time to understand and present the impact of your actions.
An important new part of the IRS requirements is to evaluate the impact of the actions you took to address the significant health needs from your previous
CHNA report. Evaluating the outcomes and impacts of these actions will help you assess how to best prioritize health needs moving forward.
Click on an item below for details:
-
Option 1: No Existing Evaluation Framework
-
If you didn't create an evaluation framework to assess progress you have made on prioritized health needs in your previous CHNA & Implementation Strategy, don't worry. This component was not required by the IRS prior to the most recent 2014 guidelines. Have a look at the Build a Plan and Evaluation Framework tab in the Design section of this guide to see examples of indicators and outcomes that you should reference when assessing the progress you have made on significant health needs identified in your previous CHNA.
You can also use the Build a Plan and Evaluation Framework section to ensure you can easily track the progress you will make on the health priorities that you choose to address in your current CHNA cycle.
See our sample evaluation framework
Important Note for Hospitals:
While you do not have to submit your evaluation framework to the IRS, in your next CHNA cycle you DO have to report your progress on the priority health needs you addressed in your Implementation Strategy. Creating an evaluation framework will make it much easier for you to clearly identify that progress in your next CHNA.
-
Option 2: Have an Existing Evaluation Framework
-
You can use your existing evaluation framework to assess the progress you have made on the health needs you chose to address in your last Implementation Strategy.
-
Tips for the Final Report
-
In your CHNA, incorporate any data you may have on the outputs, targets, and outcomes associated with each health need you chose to address in your immediately preceding CHNA & Implementation Strategy. This information can be used to help assess which health needs you choose to address in your next CHNA and Implementation Strategy. For example, if you notice that the actions you took to address a particular health need seem to have had a limited impact on improving health outcomes, you may want to choose to address that health need utilizing a different program or promising practice.
-
From the IRS
-
An evaluation of the impact of any actions that were taken, since the hospital facility finished conducting its immediately preceding CHNA, to address the significant health needs identified in the hospital facility's prior CHNA(s).
IRS Community Health Needs Assessment Rule 12/31/14
Prioritize Health Needs
After you have assessed the health needs of your community and identified the significant health needs, you are ready to prioritize these needs.
Though there may be many significant health needs in your community, your hospital might only have the capacity to address a subset of these needs. To successfully prioritize the significant health needs, establish criteria to determine a priority health need and implement a process to systematically apply those criteria.
Click on an item below for details:
-
Step 1: Set Criteria for Prioritized Health Needs
-
Establish which criteria participants should use to prioritize health needs before you begin. Here are some examples of criteria that can be used to prioritize:
- Alignment with facility’s strengths/priorities/mission
- Magnitude - number of people impacted by problem
- Severity - the rate or risk of morbidity and mortality
- Opportunity to intervene at prevention level
- Opportunity for partnership
- Addresses disparities of subgroups
- Existing resources and programs to address problem
- Solution could impact multiple problems
- Feasibility of intervention
- Availability of evidence-based approaches
- Importance of problem to community
- Economic burden on community
- Consequences of not intervening
- Evaluation results on the impact of actions taken to address the health need since your immediately preceding CHNA
Important Note for Hospitals:
The IRS requires that community input must be taken into consideration for prioritizing significant health needs from the following three groups: a) at least one representative of a state, regional or local governmental health department with knowledge of the health needs of the community; b) members of medically underserved, low-income, and minority populations in the community served by the hospital facility, or individuals or organizations serving or representing the interests of such populations; and c) written comments received on the hospital facility's most recently conducted CHNA and most recently adopted implementation strategy.
IRS Community Health Needs Assessment Rule 12/31/14
-
Step 2: Explore and Choose Prioritization Method
-
The following prioritization methods are examples of the types of different processes for you and your community to use.
Quick and simple method that works well with large groups. Individuals are given a set number of dots (stickers) and vote for the needs that they believe meet the established criteria.
Learn More
Great method to narrow a lot of options down to a few by allowing individuals to vote for a set number of topics in each round. After each round is completed, only the top results are included in the next round.
Learn More
Ideal method for small groups of decision makers who have a deep knowledge of selection criteria. This method includes generating topics, recording topics, discussing topics and then voting on topics.
Learn More
Good method for using only two criteria and with groups of decision makers who have a deep knowledge of the criteria and the issues. The strategy grid allows decision makers to focus on topics that will have the best results.
Learn More
Good for small to medium sized groups who are using multiple criteria to select priorities. In this method participants systematically analyze each priority based on the criteria.
Learn More
An advanced method where participants compare pairs of health needs based on different criteria using a matrix.
Learn More
A complex method that incorporates baseline data into an objective analysis of the criteria and the different health needs.
Learn More
Other Useful Resources
Sample prioritization worksheet from the CDC
Mind Tools
-
Tips for the Final Report
-
Make sure to document the prioritization process and criteria that you used and include the results.
-
From the IRS
-
These proposed regulations require the CHNA report to include prioritized description of the significant health needs of the community identified through the CHNA, along with a description of the process and criteria used in identifying certain health needs as significant and prioritizing those significant health needs.
IRS Community Health Needs Assessment Rule 12/31/14
Choose Needs to be Addressed
Designing your Implementation Strategy: It's time to craft a plan to take action! Start by identifying the significant health needs you will address.
Click on an item below for details:
-
Step 1: Choose Significant Needs to Address
-
In the assess and prioritize phases, you identified the significant health needs in your community and prioritized the needs that are the most important to you, your organization and your community. However, your capacity as an organization may prevent you from implementing programs that address all significant health needs.
Use the results from your prioritization session to select the list of needs you plan to address.
Quick Tip: More isn't always better! You may find it more prudent to focus your resources on a few key issues, develop a solid evaluation plan, and demonstrate impact that can be replicated with other priorities in the future.
-
Step 2: Justify Significant Needs You Don't Plan to Address
-
Provide a justification or explanation for significant needs in your community that you do not plan to address.
Here are a few sample justifications to consider:
- Other needs deemed a higher priority to address (look to prioritization outcomes)
- Issue being addressed by other facilities or organizations in the community
- Hospital does not have expertise/competencies to address the issue effectively
- Insufficient resources (financial/personnel)
- Lack of evidence-based interventions
- Issue not a priority for community members
Important Note for Hospitals:
In explaining why it does not intend to address a significant health need for purposes of paragraph (c)(1)(ii) of this section, a brief explanation of the hospital facility's reason for not addressing the health need is sufficient. Such reasons may include, for example, resource constraints, other facilities or organizations in the community addressing the need, a relative lack of expertise or competency to effectively address the need, the need being a relatively low priority, and/or a lack of identified effective interventions to address the need.
IRS Community Health Needs Assessment Rule 12/31/14
Set Goals, Determine a Strategy, and Set Objectives
After determining which needs you will address, you’ll need to set goals, pick a strategy, and set objectives for each need.
It's important to review and address the range of social, economic and physical determinants as well as individual factors that impact each health outcome. You’ll also need to make sure your team has the right skills to implement the strategy and that the specific strategy contributes to your overall goal and objectives.
Example Strategies:
- Increase public education / awareness about good nutrition
- Increase student education / awareness about reproductive health; Increase access to condoms
- Encourage senior centers and community clinics to promote flu shots
Click on an item below for details:
-
Step 1: Set Goals
-
A goal is a broad statement of a desired, long-term outcome. The goal drives all program activities.
To set goals, you’ll need to work with your partners to make sure everyone agrees upon intended results.
Example Goals:
- To reduce obesity in adults and children
- To improve the reproductive health of adolescents
- To reduce the death rate due to influenza and pneumonia
-
Step 2: Pick a Team for Each Strategy
-
When compiling a team for each strategy consider including the following people:
- Individuals within the hospital already working on this topic
- Individuals with knowledge and expertise in this topic
- Individual's ability to take on new projects/work
- Individual’s capacity to collaborate
- Health department leaders
- FQHC staff
- Non-Profit and Community Based Organization Leaders
-
Step 3: Research Strategy Options
-
Given your skills, experience and capacity, think about the type of approach that would be most effective at addressing the identified need (e.g screening, improving access, promoting awareness, advocating, providing policy support, etc.).
Conduct a broad search for a particular area of need.
Begin by selecting only one topic area. If the search produces many results then start filtering your options by selecting specific rankings (evidence-based and effective practice), primary target area of interest, additional subtopic areas, and a geography that is similar to yours. Start broad and slowly narrow your search. You don’t want to miss valuable programs by creating too many filters.
Explore Promising Practices
Take advantage of a meta analysis that has already been conducted for you!
The Centers for Disease Control and Prevention Taskforce has conducted a systematic review of a wealth of community health improvement literature and has deemed certain programs/policies most effective. These programs are tagged with a "CDC" label in the Promising Practices database. To limit your results to these programs/policies check the "CDC Community Guide" and a topic area of your choice.
Browse CDC Community Guides
List feasible and appropriate programs for your circumstance. What are the themes? Are there similar components to evidence-based programs? Are there programs in your community that are already in place that can be enhanced to be evidence-based? Make notes about programs you’d like to research further and take advantage of the contact information available to you.
Your hospital and partners may already be implementing programs and activities that have the same goal and objectives. Talk to department leaders, executives (or executive team), and community benefit staff (or team) to compile a comprehensive list of what is already taking place.
-
Step 4: Choose Strategies
-
Create a list of the programs and activities that will best contribute to your goals, are realistic for you and your partners to implement, and closely align with your organization's strengths and resources.
-
Step 5: Set Objectives
-
Objectives are specific statements detailing the desired accomplishments of a program, and are used to inform the program’s short-term outcomes. Your program should include between 1-5 objectives that can be measured by you and your team, using data you collect through your program activities. Strive to write "SMART" (Specific, Measurable, Achievable, Relevant and Time-specific) objectives that specify who, what, when and by how much. Include action verbs such as establish, increase, reduce, and create.
Quick Tip for Hospitals: Use three-year time frames so that your objectives align with the IRS’s 3-year CHNA cycle.
Example Objectives:
- By end of FY 2022, Hospital A will increase the percentage of adults who participated in the nutrition education series and reported eating 5+ servings of fruits and vegetables per day by 15%.
- By end of FY 2022, Hospital A will increase the proportion of adolescents in participating schools using condoms by 30%.
- By end of FY 2022, Hospital A will increase the percentage of adults aged 65+ participating in Program A that receive a flu vaccine by 10%.
Learn More
Design an Implementation Plan & Evaluation Framework
The goal of an implementation plan and evaluation framework is to have a clear guide for what you plan to do, how you plan to do it, who will do it, and when. This section outlines the main steps for building an evaluation framework. For more guidance overall on conducting an evaluation, check out the Conduent Healthy Communities Institute Evaluation Guide.
The last step in the community health needs assessment process is to build your plan and evaluation framework to guide you through implementing community health improvement activities.
Click on an item below for details:
-
Step 1: Define Activities
-
You've already chosen the best strategy(ies) to address each significant health need and now you'll need to create a detailed list of each specific activity that you will implement. Activities are the actions carried out by a program to accomplish its objectives. Determine what type of activities (example: education, advocacy, media campaign, funding existing efforts, etc.) would be most effective at addressing the identified need. Are there successful practices already in place that can be expanded? Are there other effective, evidence-based strategies to consider implementing? Which activities will you implement in order to achieve your objectives?
Example Activities
- Conduct nutrition education series for overweight and obese adults
- Create educational brochures and distribute to community health clinics and local schools
- Develop partnerships with senior centers and community clinics
-
Step 2: Identify Resources
-
What resources will the hospital commit to the program to achieve its goal and objectives? Make sure to include human resources (staff, providers), organizational resources (partnerships, coalitions), financial resources (grants, salaries) and material resources (computers, offices, printed materials). What is your hospital's budget and who are the best/appropriate community partners that you will work with to implement community-based activities?
Example Resources
- Hospital Nutrition Program personnel, Marketing Department personnel, printed materials, $10,000 over 3-years, local employers
- United Way, condoms, HIV test kits, birth control pills, Counseling and Testing personnel, community clinics, schools
- Hospital's Infectious Disease team, senior centers, community clinics, flu vaccination supplies
-
Step 3: Identify Outputs
-
Outputs are direct results of program activities, and help indicate whether the program was delivered to the intended audience at the intended dose. Data used to measure outputs is collected by you and your team (i.e., at the program level). Output indicators are collected at the program level and are usually a number (as opposed to a percent).
Examples Output Indicators
- # adults who participated in nutrition education series, # educational sessions conducted
- # educational brochures developed, # educational brochures distributed
- # partnerships developed with senior centers, # partnerships developed with community clinics
In order to collect the data you will also need a data source. Since outputs are the direct results of your program activities, the data typically comes from program or hospital records. Your team will need to establish a system for collecting this data.
Quick Tip: Within your implementation strategy work group, you will want to further identify the process for data collection. Which individual(s) will be responsible for collecting the raw data? Who will be responsible for reviewing and analyzing the data?
-
Step 4: Set Targets
-
To track progress with your activities, you'll want to know the current value of the indicator and set targets. Your target value should be derived from baseline or historical data (e.g., if 88 adults participated in the prior year, and the hospital is adding a new component to increase participation rates, how many adults do you expect to participate in the next year?) If this is a new program or historical data does not exist, do your best to come up with an educated guess about what the hospital can realistically accomplish given the scope of the activity and partnerships involved.
Quick Tip: If you used an evidence-based program from the promising practices database, take a look at the program results. For example, if a program demonstrated an increase in breast cancer screenings by 20%, you may want to use that number as a guide in setting your target.
-
Step 5: Set Short-Term Outcomes
-
Short-term outcomes are the short-term results of your activities and usually measure specific changes in program participant's behavior, knowledge, skills and status. Data used to measure short-term outcomes is collected by you and your team (i.e., at the program level). Short-term outcomes should be tied directly to your objectives.
To measure the short-term outcomes, you'll need to create the short-term outcome indicators which measure specific changes in program participant's behavior, knowledge and skills.
Examples of Short-Term Outcomes
- % of adults participating in program that report eating 5+ servings of fruits and vegetables per day
- % of adolescents participating in program that report using condoms
- % of adults aged 65+ living at partnering senior centers that report getting a flu shot
Quick Tip: Use one-year time frames for short-term outcomes so that progress can be reported to the IRS annually.
See an example of how Memorial Hospital of South Bend sets targets and tracks outcome measures for their priorities.
-
Step 6: Set Long–Term Outcomes
-
Long-term outcomes refer to the long-term changes we expect in health status, such as reduced disease incidence, reduced mortality and improved health. Data used to measure long-term outcomes are collected at the population level by state and national agencies (state health departments, Centers for Disease Control, etc). Long-term outcomes should be tied directly to your goal.
Quick Tip: Use timeframes that align with national or state goals for health promotion and disease prevention, such as Healthy People 2030.
To measure the long-term outcomes, you'll need create the long-term outcome indicator which measures changes we expect to see in health status. Use indicators from the community dashboard or other national/state-level data sources.
Examples of Long–Term Outcomes
- % of adults who are overweight or obese
- Chlamydia incidence rate (cases per 100,000 population)
- Age-adjusted death rate due to influenza and pneumonia (deaths per 100,000 population)
-
Step 7: Create the Framework (i.e. put it all together)
-
Now you are ready to put all the information together into one framework!
The way your plan is organized can make a big difference. Consider using this sample framework as a start and adjust as needed for your group. Make sure you clearly show the resources, outputs, and short and long-term outcomes for each of your programs. These are the essential building blocks of evaluating your plan and measuring your impact.
Once you have designed your framework for each significant need, provide a narrative to accompany the information. For a deeper explanation and examples of each of the framework components, see University of Kansas Community Toolbox.
Quick Tip: Start by filling out the fields that are known. Then, assess what's missing, plan and acquire the necessary information and return to the framework once you're ready. You will likely make many adjustments along the way.
Remember that you are working towards building a framework for addressing health needs, identifying your short and long-term outcomes, and making sure you are achieving what you set out to do. Be prepared to adjust your implementation strategy on an ongoing basis by adapting the lessons you learn along the way.
Important Note for Hospitals:
Remember, hospitals are not required to submit their Evaluation Frameworks to the IRS. Instead, they are required to evaluate the progress they have made on the health needs they chose to address in their immediately preceding CHNA & Implementation Strategy in each subsequent CHNA. Having a clear Evaluation Framework in place will ensure you are able to easily and accurately measure the progress you have made in addressing priority health needs for each CHNA.
IRS Checklist for Community Health Needs Assessment and Implementation
Strategy Requirements
Here’s a quick checklist to make sure you have all the necessary components for a successful community health needs assessment and implementation strategy as required by the IRS Community Health Needs Assessment Rule 12/31/14.*
The final report must include the following:
-
A definition of the community served by the hospital facility and a description of how the community was determined
-
A description of the process and methods used to conduct the CHNA, including identification of information gaps that limit the hospital facility's ability to assess the community's health needs
-
A description of how the hospital facility solicited and took into account input received from persons who represent the broad interests of the community it serves
-
A prioritized description of the significant health needs of the community identified through the CHNA, along with a description of the process and criteria used in identifying certain health needs as significant and prioritizing those significant health needs
-
A description of the resources potentially available to address the significant health needs identified through the CHNA
-
An evaluation of the impact of any actions that were taken, since the hospital facility finished conducting its immediately preceding CHNA, to address the significant health needs identified in the hospital facility's prior CHNA(s)
-
Board approval, or equivalent
The Implementation Strategy must include the following for all significant health needs identified in the CHNA:
- A description on how the hospital facility plans to address the health need; or
- An explanation on why the hospital facility does not intend to address the health need
- For each health need that you plan to address you will need to include the following:
- A description of the actions the hospital facility intends to take to address the health need and the anticipated impact of these actions
- A description of the resources the hospital facility plans to commit to address the health need
- A description of any planned collaboration between the hospital facility and other facilities or organizations in addressing the health need
- Board approval, or equivalent
 If comparing to other counties, these indicators will have the red, yellow, and green divided gauge. When the needle is in the green, he selected county’s value is the top best half (50%). When the needle is in the yellow, the selected county’s value is in the bottom worst half (50%). And when the needle is in the red, the selected county's value is in the worst quartile (25%) of all counties.
If comparing to other counties, these indicators will have the red, yellow, and green divided gauge. When the needle is in the green, he selected county’s value is the top best half (50%). When the needle is in the yellow, the selected county’s value is in the bottom worst half (50%). And when the needle is in the red, the selected county's value is in the worst quartile (25%) of all counties. 
 If comparing to a state or national value, these indicators will have a diamond-shaped single value icon. The arrow in the icon indicates if the indicator value is higher than, lower than or relatively equal to a state or national value. A green-colored icon represents the indicator value is better than the comparison value. A red-colored icon represents the indicator value is worse than the comparison value.
If comparing to a state or national value, these indicators will have a diamond-shaped single value icon. The arrow in the icon indicates if the indicator value is higher than, lower than or relatively equal to a state or national value. A green-colored icon represents the indicator value is better than the comparison value. A red-colored icon represents the indicator value is worse than the comparison value.