Design an Implementation Plan & Evaluation Framework
The goal of an implementation plan and evaluation framework is to have a clear guide for what you plan to do, how you plan to do it, who will do it, and when. This section outlines the main steps for building an evaluation framework. For more guidance overall on conducting an evaluation, check out the Conduent Healthy Communities Institute Evaluation Guide.
The last step in the community health needs assessment process is to build your plan and evaluation framework to guide you through implementing community health improvement activities.
Click on an item below for details:
-
Step 1: Define Activities
-
You've already chosen the best strategy(ies) to address each significant health need and now you'll need to create a detailed list of each specific activity that you will implement. Activities are the actions carried out by a program to accomplish its objectives. Determine what type of activities (example: education, advocacy, media campaign, funding existing efforts, etc.) would be most effective at addressing the identified need. Are there successful practices already in place that can be expanded? Are there other effective, evidence-based strategies to consider implementing? Which activities will you implement in order to achieve your objectives?
Example Activities
- Conduct nutrition education series for overweight and obese adults
- Create educational brochures and distribute to community health clinics and local schools
- Develop partnerships with senior centers and community clinics
-
Step 2: Identify Resources
-
What resources will the hospital commit to the program to achieve its goal and objectives? Make sure to include human resources (staff, providers), organizational resources (partnerships, coalitions), financial resources (grants, salaries) and material resources (computers, offices, printed materials). What is your hospital's budget and who are the best/appropriate community partners that you will work with to implement community-based activities?
Example Resources
- Hospital Nutrition Program personnel, Marketing Department personnel, printed materials, $10,000 over 3-years, local employers
- United Way, condoms, HIV test kits, birth control pills, Counseling and Testing personnel, community clinics, schools
- Hospital's Infectious Disease team, senior centers, community clinics, flu vaccination supplies
-
Step 3: Identify Outputs
-
Outputs are direct results of program activities, and help indicate whether the program was delivered to the intended audience at the intended dose. Data used to measure outputs is collected by you and your team (i.e., at the program level). Output indicators are collected at the program level and are usually a number (as opposed to a percent).
Examples Output Indicators
- # adults who participated in nutrition education series, # educational sessions conducted
- # educational brochures developed, # educational brochures distributed
- # partnerships developed with senior centers, # partnerships developed with community clinics
In order to collect the data you will also need a data source. Since outputs are the direct results of your program activities, the data typically comes from program or hospital records. Your team will need to establish a system for collecting this data.
Quick Tip: Within your implementation strategy work group, you will want to further identify the process for data collection. Which individual(s) will be responsible for collecting the raw data? Who will be responsible for reviewing and analyzing the data?
-
Step 4: Set Targets
-
To track progress with your activities, you'll want to know the current value of the indicator and set targets. Your target value should be derived from baseline or historical data (e.g., if 88 adults participated in the prior year, and the hospital is adding a new component to increase participation rates, how many adults do you expect to participate in the next year?) If this is a new program or historical data does not exist, do your best to come up with an educated guess about what the hospital can realistically accomplish given the scope of the activity and partnerships involved.
Quick Tip: If you used an evidence-based program from the promising practices database, take a look at the program results. For example, if a program demonstrated an increase in breast cancer screenings by 20%, you may want to use that number as a guide in setting your target.
-
Step 5: Set Short-Term Outcomes
-
Short-term outcomes are the short-term results of your activities and usually measure specific changes in program participant's behavior, knowledge, skills and status. Data used to measure short-term outcomes is collected by you and your team (i.e., at the program level). Short-term outcomes should be tied directly to your objectives.
To measure the short-term outcomes, you'll need to create the short-term outcome indicators which measure specific changes in program participant's behavior, knowledge and skills.
Examples of Short-Term Outcomes
- % of adults participating in program that report eating 5+ servings of fruits and vegetables per day
- % of adolescents participating in program that report using condoms
- % of adults aged 65+ living at partnering senior centers that report getting a flu shot
Quick Tip: Use one-year time frames for short-term outcomes so that progress can be reported to the IRS annually.
See an example of how Memorial Hospital of South Bend sets targets and tracks outcome measures for their priorities.
-
Step 6: Set Long–Term Outcomes
-
Long-term outcomes refer to the long-term changes we expect in health status, such as reduced disease incidence, reduced mortality and improved health. Data used to measure long-term outcomes are collected at the population level by state and national agencies (state health departments, Centers for Disease Control, etc). Long-term outcomes should be tied directly to your goal.
Quick Tip: Use timeframes that align with national or state goals for health promotion and disease prevention, such as Healthy People 2030.
To measure the long-term outcomes, you'll need create the long-term outcome indicator which measures changes we expect to see in health status. Use indicators from the community dashboard or other national/state-level data sources.
Examples of Long–Term Outcomes
- % of adults who are overweight or obese
- Chlamydia incidence rate (cases per 100,000 population)
- Age-adjusted death rate due to influenza and pneumonia (deaths per 100,000 population)
-
Step 7: Create the Framework (i.e. put it all together)
-
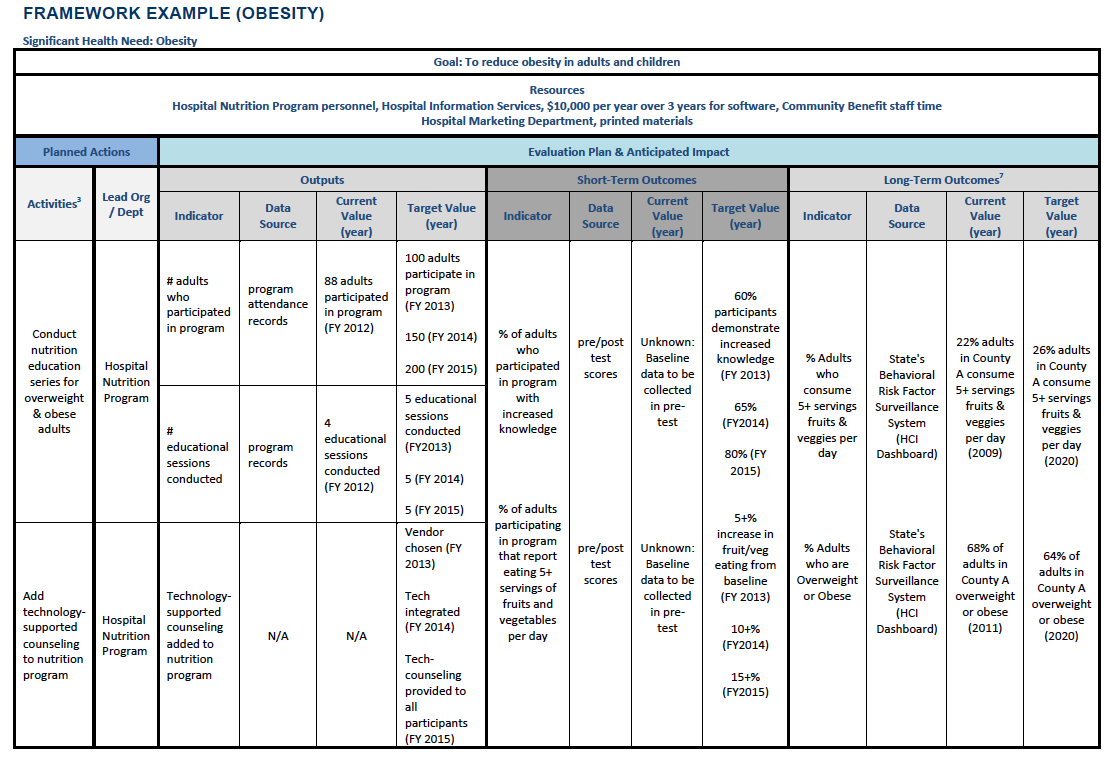
Now you are ready to put all the information together into one framework!
The way your plan is organized can make a big difference. Consider using this sample framework as a start and adjust as needed for your group. Make sure you clearly show the resources, outputs, and short and long-term outcomes for each of your programs. These are the essential building blocks of evaluating your plan and measuring your impact.
Once you have designed your framework for each significant need, provide a narrative to accompany the information. For a deeper explanation and examples of each of the framework components, see University of Kansas Community Toolbox.
Quick Tip: Start by filling out the fields that are known. Then, assess what's missing, plan and acquire the necessary information and return to the framework once you're ready. You will likely make many adjustments along the way.
Remember that you are working towards building a framework for addressing health needs, identifying your short and long-term outcomes, and making sure you are achieving what you set out to do. Be prepared to adjust your implementation strategy on an ongoing basis by adapting the lessons you learn along the way.
See an Example: Huntington Hospital (see page 41)
Important Note for Hospitals:
Remember, hospitals are not required to submit their Evaluation Frameworks to the IRS. Instead, they are required to evaluate the progress they have made on the health needs they chose to address in their immediately preceding CHNA & Implementation Strategy in each subsequent CHNA. Having a clear Evaluation Framework in place will ensure you are able to easily and accurately measure the progress you have made in addressing priority health needs for each CHNA.
Have Questions? Contact Us